
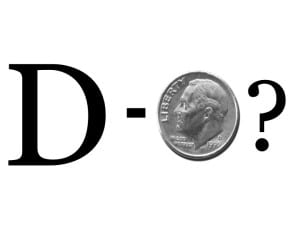
Let me save you the suspense – there is no breaking news here. There is no clear answer to the D. Dimer question/debate. It’s confusing test to order.
Why? It’s non-specific. Period. Plus, what we think we know is dangerous.
“It ain’t what you don’t know that gets you into trouble.
It’s what you know for sure that just ain’t so.”
Mark Twain
We believe if the D. Dimer is negative, there is no clot. But, we know there is some confusion here. This is only valid (as the “experts” tell me) if I use pre-test probability with the D. Dimer. A low pretest probability with a negative D. Dimer effectively rules out a PE.
But, how sensitive is a D. Dimer?
• Abnormal 95%. BUT… that’s with ELISA. What does your facility use?
• Drops to 90% with rapid ELISA and latex agglutination
• Drops to 86% with semi-quantitative latex agglutination
• Drops to 82% erythrocyte agglutination
• With sub-segmental PE-D.Dimers are abnormal in only 50% with quantitative latex agglutination.
So… 50% of the time with a small PE, I can have a negative D. Dimer!
So, once again, there is no clear-cut answer about the D. Dimer.
What is clear is that PE must be thought about with every patient with CP or SOB. This needs to be on your chart that PE was considered and ruled out 100% of the time. 100% of the time. Yep, your bronchitis. Asthmatic. Pneumonia.
The million-dollar question is: how do we rule it out? D. Dimer? Well’s? PERC? CTA? Or, could it be with weighing risk factors (Virchow’s Triad) and pertinent negative and positives?
That’s what I do. I always consider it. It’s constantly on my mind and I document that. PE is a sneaky and lethal diagnosis.
Professional feedback on this post is appreciated. What do you do? How do you use D. Dimers?
 1-800-263-6840
1-800-263-6840 Info@CME4LIFE.com
Info@CME4LIFE.com.png)
.png)














![How to Handle Emergencies more Efficiently [infographic]](https://cme4life2019.wpenginepowered.com/wp-content/uploads/2017/06/How-to-Handle-Emergencies-More-Efficiently_500px.jpg)